What is Dialectical Behavioural Therapy (DBT)?
Dialectical behaviour therapy (DBT) is a structured form of psychotherapy developed to help individuals struggling with intense emotional responses. Over the years, DBT has evolved and shown effectiveness in treating various conditions, including PTSD, depression, anxiety, and self-harming behaviours.
How DBT Can Be Effective in PTSD?
Post-Traumatic Stress Disorder often involves intense emotions, intrusive thoughts, and difficulty coping with distressing memories. Traditional trauma-focused therapies focus primarily on processing the traumatic event itself, but many individuals also need tools to manage overwhelming emotions and maintain stability in daily life. This is where Dialectical Behaviour Therapy (DBT) can play a critical role.
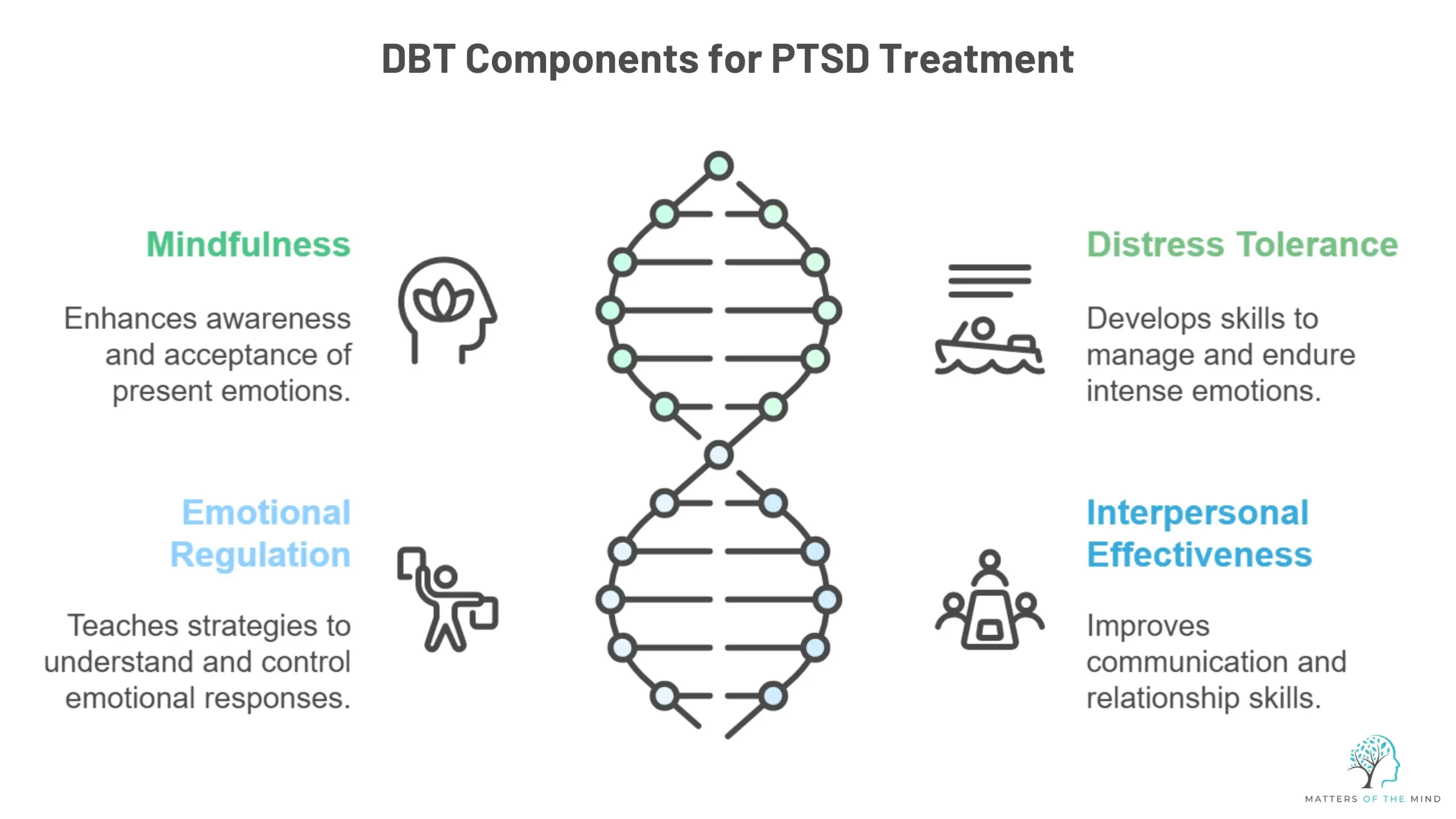
1. Mindfulness
2. Distress tolerance
3. Emotional regulation
4. Interpersonal effectiveness
Who Can Most Benefit From DBT?
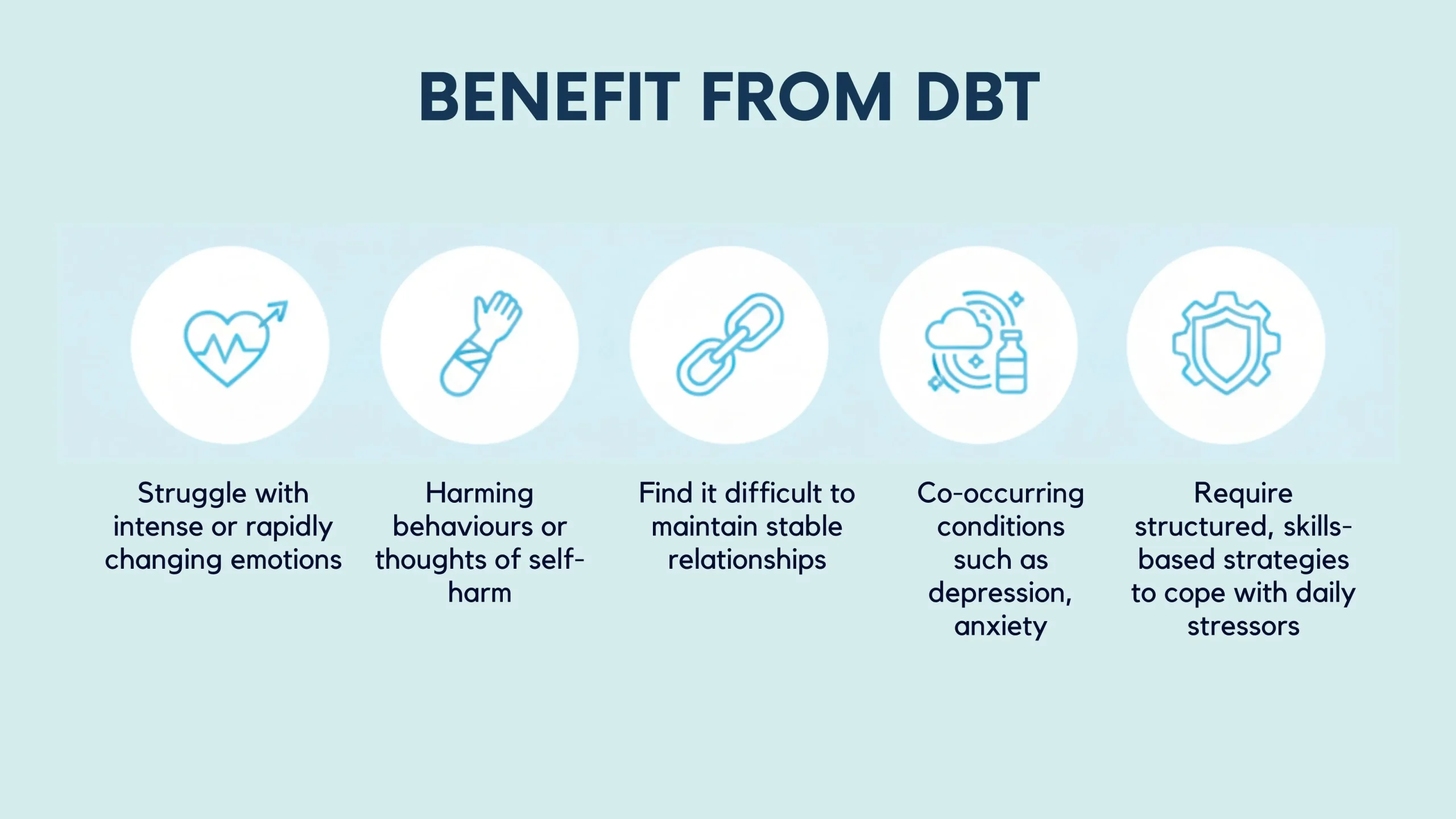
- Struggle with intense or rapidly changing emotions
- Experience self-harming behaviors or thoughts of self-harm
- Find it difficult to maintain stable relationships
- Have co-occurring conditions such as depression, anxiety, or substance misuse
- Require structured, skills-based strategies to cope with daily stressors
Is DBT actually supportive of PTSD?
Research has increasingly demonstrated that DBT can be beneficial for individuals experiencing PTSD, particularly when symptoms are compounded by emotional dysregulation or self-harming behaviors. Studies indicate that incorporating DBT into PTSD treatment can lead to:
- Reduced frequency and intensity of flashbacks and intrusive thoughts
- Improved emotion regulation and coping strategies
- Decreased self-harm and impulsive behaviors
- Enhanced ability to engage in daily life and relationships
Final Thoughts
Living with PTSD can feel challenging, but recovery is possible with the right support and therapeutic approach. Dialectical behaviour therapy offers more than just coping mechanisms, rather it provides individuals with a structured set of skills to navigate these emotions, build resilience and strengthen relationships. By combining acceptance with change, DBT empowers individuals to regain a sense of stability and control in their lives.
If you or someone you know is struggling with PTSD and would like to explore supportive therapies such as DBT, you can reach out to Dr Kavita Deepak-Knights, a trusted mental health psychologist based in Windsor, Berkshire. Her compassionate, evidence-based approach can help guide you toward recovery and improved well-being.